
Healthcare Fraud Detection Market Report by Component (Software, Services), Type (Descriptive Analytics, Predictive Analytics, Prescriptive Analytics), Delivery Mode (On-premises, On-demand), Application (Insurance Claims Review, Payment Integrity), End User (Private Insurance Payers, Government Agencies, and Others), and Region 2025-2033
Global Healthcare Fraud Detection Market:
The global healthcare fraud detection market size reached USD 3.0 Billion in 2024. Looking forward, IMARC Group expects the market to reach USD 16.4 Billion by 2033, exhibiting a growth rate (CAGR) of 19.66% during 2025-2033. The rising incidence of healthcare fraud, ongoing technological advancements, healthcare digitalization, and adoption of cloud-based solutions are primarily driving the market's growth.
|
Report Attribute
|
Key Statistics
|
|---|---|
|
Base Year
|
2024
|
|
Forecast Years
|
2025-2033
|
|
Historical Years
|
2019-2024
|
|
Market Size in 2024
|
USD 3.0 Billion |
|
Market Forecast in 2033
|
USD 16.4 Billion |
| Market Growth Rate (2025-2033) | 19.66% |
Healthcare Fraud Detection Market Analysis:
- Major Market Drivers: Due to an increase in the number of patients seeking health insurance, there is a rise in the demand for healthcare fraud detection solutions. This, along with the growing prepayment review model in the healthcare industry, represents one of the key factors driving the market. Moreover, the increasing number of pharmacy claims-related frauds across the globe is propelling the healthcare fraud detection market growth.
- Key Market Trends: The rising demand for solutions that have biometric sensors to identify frauds coupled with the growing adoption of healthcare fraud analytics, especially in developing countries, is positively influencing the healthcare fraud detection market size. Moreover, the increasing returns on investment (ROI), rising use of social media, and funding for the implementation of information technology (IT) platforms are bolstering the healthcare fraud detection market share.
- Competitive Landscape: Some of the prominent healthcare fraud detection market companies include CGI Inc., Conduent Inc., ExlService Holdings Inc., Fair Isaac Corporation, HCL Technologies Limited, International Business Machines Corporation, Northrop Grumman Corporation, RELX Group plc, SAS Institute Inc., UnitedHealth Group, and Wipro Ltd., among many others.
- Geographical Trends: According to the healthcare fraud detection market dynamics, North America is one of the most affected regions by healthcare fraud, primarily due to the complexity of the healthcare insurance system. Moreover, European countries are investing heavily in digital healthcare transformation, with fraud detection being a key focus in healthcare IT modernization efforts.
- Challenges and Opportunities: The rising data privacy concerns and shortage of skilled workforce are hampering the market's growth. However, AI/ML-based fraud detection systems can reduce the incidence of false positives and improve accuracy by learning from historical fraud data, making them highly efficient. The growing demand for these technologies presents significant opportunities for companies providing AI-driven solutions.
Healthcare Fraud Detection Market Trends:
Rising Incidence of Healthcare Fraud
Healthcare fraud is a significant issue globally, costing billions of dollars annually. For instance, according to an article published by the National Library of Medicine, approximately US$ 455 billion of the US$ 7.35 trillion spent on healthcare globally each year is lost to fraud and corruption. There has been rising awareness and detection of various types of healthcare fraud, such as insurance claims fraud, billing for unnecessary services, and identity theft. These are pushing healthcare organizations and payers to adopt more advanced fraud detection solutions. These factors are expected to propel the healthcare fraud detection market share in the coming years.
Expanding Health Insurance Market
The global health insurance market is expanding, with more individuals getting coverage due to increased awareness and government initiatives. For instance, according to IMARC, the global health insurance market size reached USD 1,835.9 Billion in 2023. Looking forward, IMARC Group expects the market to reach USD 3,208.4 Billion by 2032, exhibiting a growth rate (CAGR) of 6.2% during 2024-2032. This expansion brings more healthcare transactions and insurance claims, creating more opportunities for fraudulent activities. As a result, insurance companies are heavily investing in fraud detection technologies to minimize financial losses. These factors further positively influence the healthcare fraud detection market growth.
Technological Innovations
AI and ML technologies are transforming healthcare fraud detection by enabling more efficient and accurate identification of fraudulent patterns and outliers. These technologies allow for real-time monitoring of claims and transactions, improving the ability to detect fraud at an early stage. For instance, in August 2024, MediBuddy, a digital healthcare platform, launched 'Sherlock', an AI-powered fraud detection system for healthcare reimbursement claims. The platform uses advanced technologies such as artificial intelligence (AI), machine learning (ML), and data analytics to detect and prevent fraudulent claims in real-time, transforming the reimbursement process for healthcare providers, insurers, and patients, thereby boosting the healthcare fraud detection market share.
Global Healthcare Fraud Detection Industry Segmentation:
IMARC Group provides an analysis of the key trends in each segment of the global healthcare fraud detection market report, along with forecasts at the global, regional, and country levels from 2025-2033. Our report has categorized the market based on component, type, delivery mode, application, and end user.
Breakup by Component:
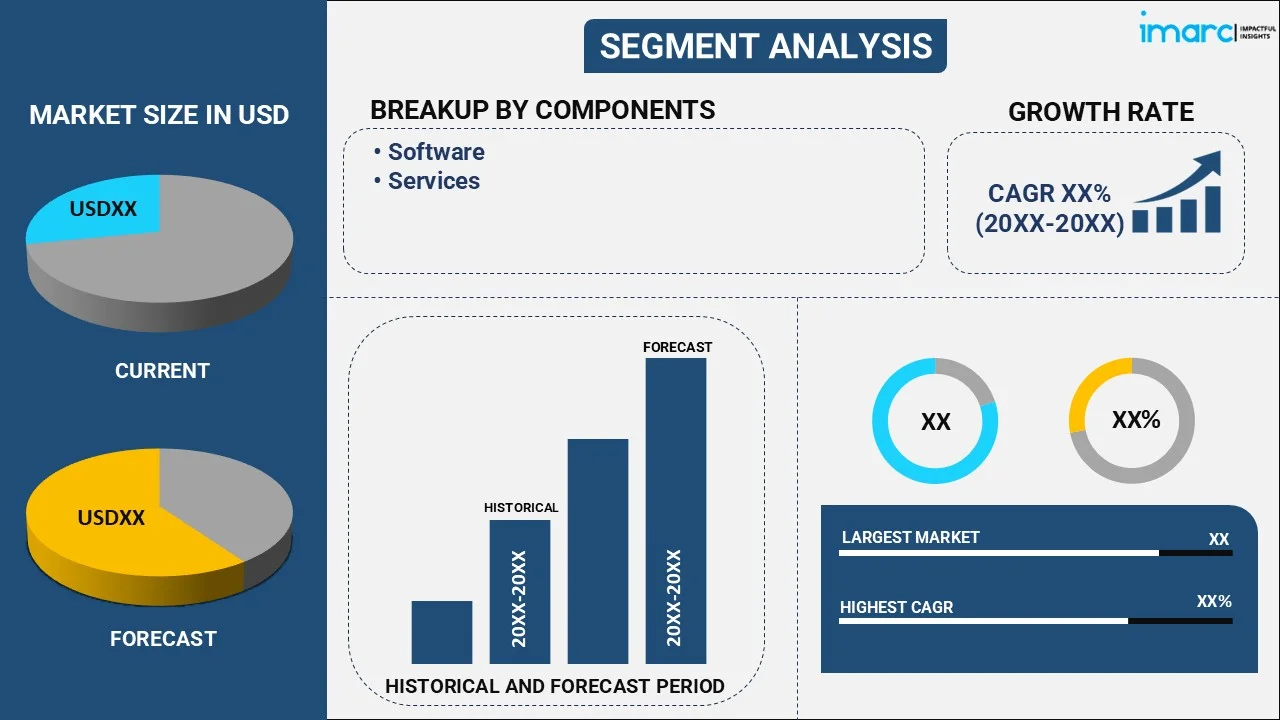
- Software
- Services
The report has provided a detailed breakup and analysis of the healthcare fraud detection market based on the component. This includes software and services.
According to the healthcare fraud detection market outlook, the increasing number of fraudulent activities in healthcare, such as false insurance claims, billing fraud, and identity theft, drives the need for sophisticated fraud detection software. Healthcare fraud costs billions of dollars annually worldwide, creating demand for solutions that can mitigate these losses. Moreover, many healthcare organizations, particularly smaller providers and insurers, lack the internal resources and expertise to manage fraud detection systems. This has created a demand for outsourcing fraud detection services to third-party specialists who can provide continuous monitoring, risk assessments, and analytics.
Breakup by Type:
- Descriptive Analytics
- Predictive Analytics
- Prescriptive Analytics
The report has provided a detailed breakup and analysis of the healthcare fraud detection market based on the type. This includes descriptive analytics, predictive analytics, and prescriptive analytics.
According to the healthcare fraud detection market overview, the increasing number of healthcare fraud cases has created a need for healthcare organizations to analyze past data and understand historical fraud patterns. Descriptive analytics helps organizations visualize fraud trends and evaluate where and how fraud has occurred. Moreover, healthcare organizations increasingly require real-time fraud detection to minimize financial losses. Predictive analytics enables real-time monitoring of claims and transactions, flagging suspicious activities for immediate review and reducing the lag between fraudulent activity and detection. Besides this, healthcare organizations need more than just predictions—they require actionable recommendations on how to respond to potential fraud. Prescriptive analytics uses optimization algorithms to suggest the best course of action, such as denying a claim, flagging it for further review, or adjusting internal fraud detection rules.
Breakup by Delivery Mode:
- On-premises
- On-demand
The report has provided a detailed breakup and analysis of the healthcare fraud detection market based on the delivery mode. This includes on-premises and on-demand.
On-premises solutions are installed and run on the healthcare organization’s internal servers and data centers. The organization maintains full control over the infrastructure, software, and data security. Moreover, healthcare organizations handling sensitive patient data are subject to stringent regulations like HIPAA in the U.S. and GDPR in Europe. On-premises solutions are often preferred by organizations that must meet strict compliance standards, as they allow full control over data storage and security. Furthermore, on-demand or cloud-based solutions are hosted on external cloud providers' servers and accessed via the internet. Healthcare organizations pay for the service based on usage, without the need to maintain internal hardware or software. On-demand solutions eliminate the need for significant upfront investments in IT infrastructure. Instead, organizations pay for fraud detection services on a subscription basis, allowing for more flexible budgeting.
Breakup by Application:
- Insurance Claims Review
- Payment Integrity
The report has provided a detailed breakup and analysis of the healthcare fraud detection market based on the application. This includes insurance claims review and payment integrity.
Insurance claims review is the process of thoroughly examining healthcare claims submitted by providers to ensure that they are accurate, legitimate, and compliant with healthcare regulations before they are paid. This process helps detect potential fraud, errors, or abusive billing practices. Moreover, payment integrity refers to ensuring that the payments made by insurers for healthcare services are accurate, appropriate, and in line with the actual care delivered. It involves identifying improper payments, preventing overpayments, and recovering funds in cases of fraud, waste, or abuse.
Breakup by End User:
- Private Insurance Payers
- Government Agencies
- Others
The report has provided a detailed breakup and analysis of the healthcare fraud detection market based on the end user. This includes private insurance payers, government agencies, and others.
Private insurance companies face increasing fraud schemes such as upcoding, unbundling, phantom billing, and medical identity theft. Fraudulent activities not only inflate healthcare costs but also erode trust between insurers, providers, and patients. The rising frequency and sophistication of fraud necessitate advanced fraud detection solutions, pushing private payers to invest in AI-driven and predictive analytics-based systems to detect and mitigate these activities in real-time. Moreover, government healthcare programs, such as Medicare and Medicaid in the U.S., handle billions of dollars in claims annually. The sheer volume of claims makes these programs highly susceptible to fraud, waste, and abuse. The large scale of these programs drives government agencies to invest heavily in fraud detection systems that can process claims at scale while identifying anomalies that indicate potential fraud. Real-time monitoring and post-payment review systems are in high demand to protect these public funds.
Breakup by Region:
- North America
- United States
- Canada
- Asia-Pacific
- China
- Japan
- India
- South Korea
- Australia
- Indonesia
- Others
- Europe
- Germany
- France
- United Kingdom
- Italy
- Spain
- Russia
- Others
- Latin America
- Brazil
- Mexico
- Others
- Middle East and Africa
The report has also provided a comprehensive analysis of all the major regional markets, which include North America (the United States and Canada); Europe (Germany, France, the United Kingdom, Italy, Spain, Russia, and others); Asia Pacific (China, Japan, India, South Korea, Australia, Indonesia, and others); Latin America (Brazil, Mexico, and others); and the Middle East and Africa.
According to the healthcare fraud detection market statistics, North America acquires a prominent share in the healthcare fraud detection market owing to high healthcare expenditures in countries like the United States. The widespread use of EHRs across Europe has led to a surge in healthcare data. As more patient information and billing processes become digitized, the risk of fraudulent activities such as false claims and identity theft rises. Fraud detection systems are being deployed to identify anomalies in these vast datasets and prevent fraudulent claims.
Competitive Landscape:
The market research report has provided a comprehensive analysis of the competitive landscape. Detailed profiles of all major market companies have also been provided. Some of the key players in the market include:
- CGI Inc.
- Conduent Inc.
- ExlService Holdings Inc.
- Fair Isaac Corporation
- HCL Technologies Limited
- International Business Machines Corporation
- Northrop Grumman Corporation
- RELX Group plc
- SAS Institute Inc.
- UnitedHealth Group
- Wipro Ltd
(Please note that this is only a partial list of the key players, and the complete list is provided in the report.)
Healthcare Fraud Detection Market Recent Developments:
- September 2024: Microblink, an AI-powered identity verification company, established its Fraud Lab, a section dedicated to boosting identity fraud detection.
- August 2024: MediBuddy, a digital healthcare platform, launched 'Sherlock', an AI-powered fraud detection system for healthcare reimbursement claims. The platform uses advanced technologies such as artificial intelligence (AI), machine learning (ML), and data analytics to detect and prevent fraudulent claims in real-time, transforming the reimbursement process for healthcare providers, insurers, and patients.
- March 2024: HealthLock, a medical fraud and overbilling prevention technology, launched its platform for commercial, small company, and consumer Mastercard cardholders in the United States.
Healthcare Fraud Detection Market Report Scope:
| Report Features | Details |
|---|---|
| Base Year of the Analysis | 2024 |
| Historical Period | 2019-2024 |
| Forecast Period | 2025-2033 |
| Units | Billion USD |
| Scope of the Report | Exploration of Historical Trends and Market Outlook, Industry Catalysts and Challenges, Segment-Wise Historical and Future Market Assessment:
|
| Components Covered | Software, Services |
| Types Covered | Descriptive Analytics, Predictive Analytics, Prescriptive Analytics |
| Delivery Modes Covered | On-premises, On-demand |
| Applications Covered | Insurance Claims Review, Payment Integrity |
| End Users Covered | Private Insurance Payers, Government Agencies, Others |
| Regions Covered | Asia Pacific, Europe, North America, Latin America, Middle East and Africa |
| Countries Covered | United States, Canada, Germany, France, United Kingdom, Italy, Spain, Russia, China, Japan, India, South Korea, Australia, Indonesia, Brazil, Mexico |
| Companies Covered | CGI Inc., Conduent Inc., ExlService Holdings Inc., Fair Isaac Corporation, HCL Technologies Limited, International Business Machines Corporation, Northrop Grumman Corporation, RELX Group plc, SAS Institute Inc., UnitedHealth Group, Wipro Ltd., etc. |
| Customization Scope | 10% Free Customization |
| Post-Sale Analyst Support | 10-12 Weeks |
| Delivery Format | PDF and Excel through Email (We can also provide the editable version of the report in PPT/Word format on special request) |
Key Benefits for Stakeholders:
- IMARC's report offers a comprehensive quantitative analysis of various market segments, historical and current market trends, market forecasts, and dynamics of the healthcare fraud detection market from 2019-2033.
- The research study provides the latest information on the market drivers, challenges, and opportunities in the global healthcare fraud detection market.
- The study maps the leading, as well as the fastest-growing, regional markets. It further enables stakeholders to identify the key country-level markets within each region.
- Porter's five forces analysis assists stakeholders in assessing the impact of new entrants, competitive rivalry, supplier power, buyer power, and the threat of substitution. It helps stakeholders to analyze the level of competition within the healthcare fraud detection industry and its attractiveness.
- The competitive landscape allows stakeholders to understand their competitive environment and provides insight into the current positions of key players in the market.
Key Questions Answered in This Report
The healthcare fraud detection market was valued at USD 3.0 Billion in 2024.
The healthcare fraud detection market is projected to exhibit a CAGR of 19.66% during 2025-2033.
The healthcare fraud detection market is driven by rising healthcare fraud incidents, stricter regulatory frameworks, and the growing need for cost containment. Advancements in AI, machine learning, and data analytics improve detection efficiency. Additionally, increasing adoption of healthcare IT systems and rising awareness of fraud risks contribute to market growth.
North America currently dominates the market driven by the increasing prevalence of healthcare fraud, stringent regulations, and the need to reduce fraudulent claims.
Some of the major players in the healthcare fraud detection market include CGI Inc., Conduent Inc., ExlService Holdings Inc., Fair Isaac Corporation, HCL Technologies Limited, International Business Machines Corporation, Northrop Grumman Corporation, RELX Group plc, SAS Institute Inc., UnitedHealth Group, Wipro Ltd., etc.
Need more help?
- Speak to our experienced analysts for insights on the current market scenarios.
- Include additional segments and countries to customize the report as per your requirement.
- Gain an unparalleled competitive advantage in your domain by understanding how to utilize the report and positively impacting your operations and revenue.
- For further assistance, please connect with our analysts.
 Request Customization
Request Customization
 Speak to an Analyst
Speak to an Analyst
 Request Brochure
Request Brochure
 Inquire Before Buying
Inquire Before Buying




.webp)




.webp)












